| [1] |
LU QY, YU SF, MENG XY, et al. microRNAs: Important regulatory molecules in acute lung injury/acute respiratory distress syndrome[J]. Int J Mol Sci, 2022, 23(10): 5545. doi: 10.3390/ijms23105545
|
| [2] |
LIU C, XIAO K, XIE LX. Advances in the use of exosomes for the treatment of ALI/ARDS[J]. Front Immunol, 2022, 13: 971189. doi: 10.3389/fimmu.2022.971189
|
| [3] |
MEYER NJ, GATTINONI L, CALFEE CS. Acute respiratory distress syndrome[J]. Lancet, 2021, 398(10300): 622-637. doi: 10.1016/S0140-6736(21)00439-6
|
| [4] |
谢璨灿, 吴双华, 李峥嵘, 等. 电针刺激通过JAK1/STAT3通路减轻脓毒症大鼠的急性肺损伤[J]. 南方医科大学学报, 2020, 40(11): 1662-1667. doi: 10.12122/j.issn.1673-4254.2020.11.20XIE CC, WU SH, LI ZR, et al. Electroacupuncture protects septic rats from acute lung injury through the JAK1/STAT3 pathway[J]. J South Med Univ, 2020, 40(11): 1662-1667. doi: 10.12122/j.issn.1673-4254.2020.11.20
|
| [5] |
LUO D, LIU L, ZHANG HM, et al. Electroacupuncture pretreatment exhibits lung protective and anti-inflammation effects in lipopolysaccharide-induced acute lung injury via SIRT1-dependent pathways[J]. Evid Based Complement Alternat Med, 2022, 2022: 2252218.
|
| [6] |
SHI XY, LI T, LIU YT, et al. HSF1 protects sepsis-induced acute lung injury by inhibiting NLRP3 inflammasome activation[J]. Front Immunol, 2022, 13: 781003. doi: 10.3389/fimmu.2022.781003
|
| [7] |
WANG H, SUN XT, LU Q, et al. The mitochondrial redistribution of eNOS is involved in lipopolysaccharide induced inflammasome activation during acute lung injury[J]. Redox Biol, 2021, 41: 101878. doi: 10.1016/j.redox.2021.101878
|
| [8] |
LI JM, BAI Y, TANG YT, et al. A 4-benzene-indol derivative alleviates LPS-induced acute lung injury through inhibiting the NLRP3 inflammasome[J]. Front Immunol, 2022, 13: 812164. doi: 10.3389/fimmu.2022.812164
|
| [9] |
XU J, LU LQ, LI LF. NEK7: A novel promising therapy target for NLRP3-related inflammatory diseases[J]. Acta Biochim Biophys Sin, 2016, 48(10): 966-968. doi: 10.1093/abbs/gmw080
|
| [10] |
SUN ZZ, GONG W, ZHANG Y, et al. Physiological and pathological roles of mammalian NEK7[J]. Front Physiol, 2020, 11: 606996. doi: 10.3389/fphys.2020.606996
|
| [11] |
刘瑞莲. 利多卡因通过P2X7R/NLRP3/Caspase-1途径对脂多糖诱导急性肺损伤大鼠的保护作用研究[D]. 广州: 广州医科大学, 2018.LIU RL. Protective effect of lidocaine on lipopolysaccharide induced acute lung injury in rat via attenuating P2X7R/NLRP3/caspase-1 pathway[D]. Guangzhou: Guangzhou Medical University, 2018.
|
| [12] |
刘心月, 苏景超, 张新芳, 等. 电针预处理对脂多糖诱导的脓毒症急性肺损伤大鼠肺组织中血管紧张素转化酶2、血管紧张素(1-7) 的影响[J]. 针刺研究, 2022, 47(8): 684-689. https://www.cnki.com.cn/Article/CJFDTOTAL-XCYJ202208005.htmLIU XY, SU JC, ZHANG XF, et al. Electroacupuncture preconditioning improves pulmonary function via inhibiting inflammatory response and up-regulating expression of ACE2 and Ang (1-7) in lipopolysaccharide-induced acute lung injury rats[J]. Acupunct Res, 2022, 47(8): 684-689. https://www.cnki.com.cn/Article/CJFDTOTAL-XCYJ202208005.htm
|
| [13] |
李忠仁. 实验针灸学[M]. 2版. 北京: 中国中医药出版社, 2007.LI ZR. Experimental Acupuncture[M]. 2nd ed. Beijing: China press of traditional Chinese medicine, 2007.
|
| [14] |
杨英伟, 李建, 刘恩顺, 等. 204例ALI/ARDS患者中医证候分布与演变特征研究[J]. 中华中医药杂志, 2015, 30(3): 911-913.YANG YW, LI J, LIU ES, et al. Study on the TCM syndrome distribution and evolution characteristic of 204 ALI/ARDS patients[J]. China J Tradit Chin Med Pharm, 2015, 30(3): 911-913.
|
| [15] |
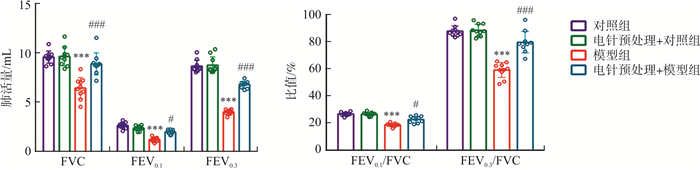
徐弋茜, 崔翔, 刘坤, 等. 电针和预电针改善急性肺损伤大鼠肺功能的效应差异[J]. 针刺研究, 2022, 47(7): 580-586. doi: 10.13702/j.1000-0607.20211299XU YQ, CUI X, LIU K, et al. Comparison of effects of routine electroacupuncture and pre-electroacupuncture in improving lung function in acute lung injury rats[J]. Acupunct Res, 2022, 47(7): 580-586. doi: 10.13702/j.1000-0607.20211299
|
| [16] |
LIU SB, WANG ZF, SU YS, et al. A neuroanatomical basis for electroacupuncture to drive the vagal-adrenal axis[J]. Nature, 2021, 598(7882): 641-645. doi: 10.1038/s41586-021-04001-4
|
| [17] |
ZHANG YG, ZHENG L, DENG HM, et al. Electroacupuncture alleviates LPS-induced ARDS through α7 nicotinic acetylcholine receptor-mediated inhibition of ferroptosis[J]. Front Immunol, 2022, 13: 832432. doi: 10.3389/fimmu.2022.832432
|
| [18] |
张毅. 电针预处理调控ALI大鼠肺泡巨噬细胞M1极化的作用研究[D]. 合肥: 安徽中医药大学, 2021.ZHANG Y. Effect of electro-acupuncture pretreatment on M1 polarization of alveolar macrophages in acute lung injury rats[D]. Hefei: Anhui University of Chinese Medicine, 2021.
|
| [19] |
AVECILLAS JF, FREIRE AX, ARROLIGA AC. Clinical epidemiology of acute lung injury and acute respiratory distress syndrome: Incidence, diagnosis, and outcomes[J]. Clin Chest Med, 2006, 27(4): 549-557. doi: 10.1016/j.ccm.2006.06.001
|
| [20] |
NOVICK D, KIM S, KAPLANSKI G, et al. Interleukin-18, more than a Th1 cytokine[J]. Semin Immunol, 2013, 25(6): 439-448. doi: 10.1016/j.smim.2013.10.014
|
| [21] |
YANG J, YANG JW, HUANG XF, et al. Glibenclamide alleviates LPS-induced acute lung injury through NLRP3 inflammasome signaling pathway[J]. Mediators Inflamm, 2022, 2022: 8457010.
|
| [22] |
DUAN YH, WANG JH, CAI J, et al. The leucine-rich repeat (LRR) domain of NLRP3 is required for NLRP3 inflammasome activation in macrophages[J]. J Biol Chem, 2022, 298(12): 102717. doi: 10.1016/j.jbc.2022.102717
|
| [23] |
SHAO BZ, XU ZQ, HAN BZ, et al. NLRP3 inflammasome and its inhibitors: A review[J]. Front Pharmacol, 2015, 6: 262.
|
| [24] |
SONG H, ZHAO CY, YU ZX, et al. UAF1 deubiquitinase complexes facilitate NLRP3 inflammasome activation by promoting NLRP3 expression[J]. Nat Commun, 2020, 11(1): 6042. doi: 10.1038/s41467-020-19939-8
|
| [25] |
ZANGIABADI S, ABDUL-SATER AA. Regulation of the NLRP3 inflammasome by posttranslational modifications[J]. J Immunol, 2022, 208(2): 286-292. doi: 10.4049/jimmunol.2100734
|
| [26] |
PAIK S, KIM JK, SILWAL P, et al. An update on the regulatory mechanisms of NLRP3 inflammasome activation[J]. Cell Mol Immunol, 2021, 18(5): 1141-1160. doi: 10.1038/s41423-021-00670-3
|
| [27] |
GUAN XX, YANG HH, ZHONG WJ, et al. Fn14 exacerbates acute lung injury by activating the NLRP3 inflammasome in mice[J]. Mol Med, 2022, 28(1): 85. doi: 10.1186/s10020-022-00514-4
|
| [28] |
ZHANG Y, LI XR, GRAILER JJ, et al. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome[J]. J Pineal Res, 2016, 60(4): 405-414. doi: 10.1111/jpi.12322
|
| [29] |
FRY AM, BAYLISS R, ROIG J. Mitotic regulation by NEK kinase networks[J]. Front Cell Dev Biol, 2017, 5: 102. doi: 10.3389/fcell.2017.00102
|
| [30] |
SHARIF H, WANG L, WANG WL, et al. Structural mechanism for NEK7-licensed activation of NLRP3 inflammasome[J]. Nature, 2019, 570(7761): 338-343. doi: 10.1038/s41586-019-1295-z
|
| [31] |
HE Y, ZENG MY, YANG DH, et al. NEK7 is an essential mediator of NLRP3 activation downstream of potassium efflux[J]. Nature, 2016, 530(7590): 354-357. doi: 10.1038/nature16959
|
| [32] |
WANG Y, ZENG Z, RAN JR, et al. The critical role of potassium efflux and Nek7 in Pasteurella multocida -induced NLRP3 inflammasome activation[J]. Front Microbiol, 2022, 13: 849482. doi: 10.3389/fmicb.2022.849482
|
| [33] |
LIU H, GU CP, LIU MJ, et al. NEK7 mediated assembly and activation of NLRP3 inflammasome downstream of potassium efflux in ventilator-induced lung injury[J]. Biochem Pharmacol, 2020, 177: 113998.
|




 下载:
下载: